The fat man of Maldon could serve as a warning: latest Essex figures prompt councils to call on doctors to tackle the obesity crisis
By The Editor 7th Sep 2021
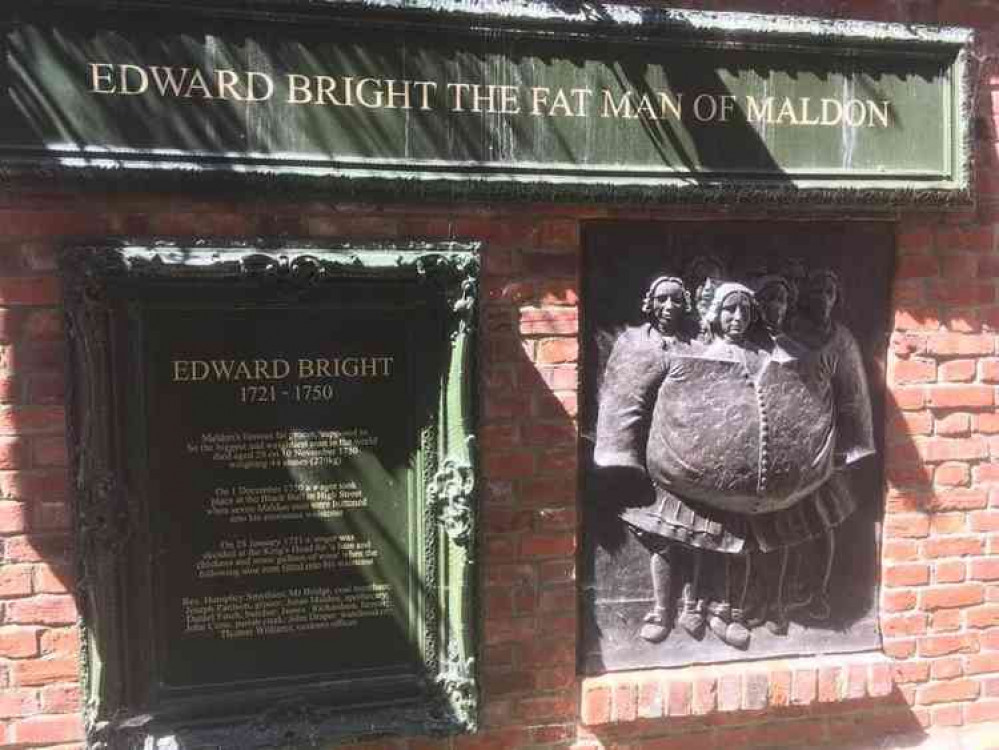
IT seems the famous 'fat man of Maldon' - Edward Bright - could serve as a warning with latest figures revealing that nearly two thirds of adults in Essex are overweight or obese.
Mr Bright, who lived and worked in the town as a grocer in the 18th Century, was famed for his tremendous size at it was very unusual at the time.
Now the body that represents local councils, the Local Government Association (LGA) is urging doctors to to be frank with obese people – ultimately helping to take pressure off stretched social services.
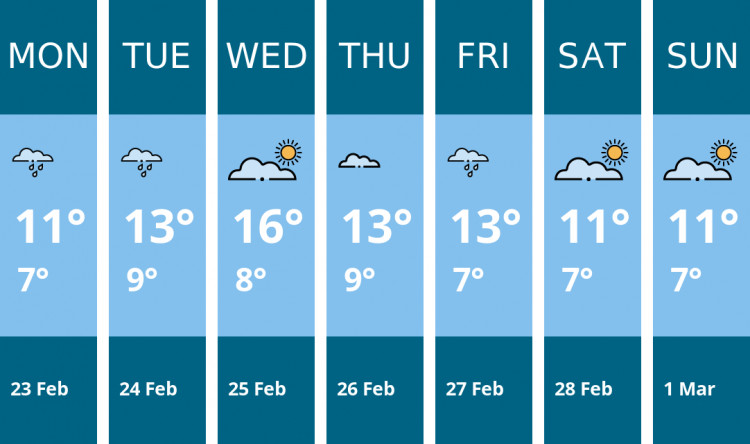
Public Health England figures show 63 per cent of adults in the county were classed in the two categories in 2018-19, the latest period for which data is available.
This was the same as the average across the East of England – but it was just above the England average of 62 per cent.
Separate figures show that 22 per cent of children aged four to five-years-old in Essex were overweight or obese in the 2018-19 academic year. Nationally up to a third of adults are predicted to be obese by 2024.Councils say a fear of causing offence and a lack of available services to help is making the problem worse
The problem of obesity has become more urgent
It says this "frank approach" has become more urgent considering that severe obesity rates have soared seven-fold for men and almost trebled for women since the mid-90s, and in light of widening health inequalities, which have seen obesity rates increase most among those from more deprived backgrounds, and among different ethnic groups. Obesity is linked to diseases including type 2 diabetes, hypertension, some cancers, heart disease, stroke, liver disease and musculoskeletal conditions. This affects people's ability to live independently, leading to increased benefit costs and demand for social care, which is already under significant stress. Research shows that the yearly cost of council funded community-based social care for a severely obese person is nearly double the cost of a person with a healthy BMI, which equates to an extra £423,000 in annual excess social care costs for a typical council. Further research shows that obese people are 25 per cent more likely to be using some form of long-term care in two years' time, than those with a healthy BMI. [H3]Obesity is a "ticking timebomb" Cllr Ian Hudspeth, Chairman of the LGA's Community Wellbeing Board, said: "Obesity is a ticking timebomb for the nation's health and is one of the most serious public health challenges of the 21st century, but its impact on adult social care is largely overlooked."Unless we tackle the stigma and serious challenge of obesity, the costly and debilitating major health conditions it causes could bankrupt adult social care and NHS services.
"Health professionals need to start having frank conversations about their people's weight if it could be an underlying cause of their condition and routinely record it; individuals need to take responsibility for their own decisions and government needs to support them to do so.
"Obesity needs to be tackled head-on, otherwise people's health will continue to suffer, health inequalities associated with obesity will remain and the economic and social costs will increase to unsustainable levels."
A spokesperson for Essex County Council, said: "We recognise the issues that being overweight and obesity can cause, not only in terms of the effect that it has on an individual's health, but also the wider effect on services that local authorities provide.
"In Essex, we commission an award-winning weight management programme – My Weight Matters – that has helped thousands of people across the county to successfully lose weight and improve their quality of life."
What do you think? How could people be better supported to lose weight and lead healthier lifestyles?
CHECK OUT OUR Jobs Section HERE!
maldon vacancies updated hourly!
Click here to see more: maldon jobs
Share: